How Smart Cookie Dog Treats got its start! And why the Survivor is our top seller!
Preserving Options
Young cancer patient forced to make fertility a present issue

At 24, Bri Pasko hadn’t thought much about children, besides assuming she’d have them one day. Then on Feb. 10, 2012, Bri jumped in the shower to begin her usual morning routine and for some reason, gave herself a breast self-examination.
“I hadn’t been good about regularly preforming self-breast exams and assumed the exams my doctor performed at my physical once a year would suffice,” says Bri. “I figured since breast cancer ran in my family, I needed to start doing them.”
In her left breast, Bri felt what no woman ever wants to feel—a hard, pea-sized lump. “I didn’t know if this was normal or not, so I instantly called my primary care provider.”
Twenty-four hours later she found herself at the doctor’s office. Because of Bri’s age and the size of the lump, her doctor didn’t know if it could be cancer. Further examinations were needed.
A mammogram couldn’t detect the lump so she was sent for an ultrasound and biopsy. Then the waiting began. A little over a week after Bri’s self-examination, the phone rang.
“My doctor called me back on a Saturday, so I instantly knew the news wasn’t positive,” Bri says. With her sister by her side, Bri listened to the news: stage I breast cancer. At less than a centimeter, the tumor had yet to spread. Bri’s self-examination had caught the cancer early.
“I always assumed if I found out I had cancer I’d immediately start crying, but I was just in shock,” Bri says. “As I listened to my doctor, I couldn’t stop shaking or process what she was saying.”
Seeking Specialized Care
Every year, 27,000 women under the age of 45 are diagnosed with breast cancer. Compared to the more than 200,000 cases in women over 45, Bri’s cancer was considered uncommon. It was also considered treatable. She’d need to have a lumpectomy and undergo six weeks of radiation.
Prior to treatment, Bri and her boyfriend, Scott Bradley, decided to get a second opinion.
After searching the internet for the best breast cancer specialists, Scott learned the University of Colorado Cancer Center had a young women’s breast cancer program. They were advised to schedule an appointment with Virginia Borges, MD, MMSC, director of the Young Women’s Breast Cancer Translational Program.
“I wanted Bri to go to the best of the best,” says Scott, admitting he researched multiple places out-of-state. “We ended up coming to the University of Colorado because of the multidisciplinary clinic and the ability to have our case reviewed by multiple physicians.”
It turns out Bri was also looking for a particular oncologist—one who didn’t see her as the average breast cancer patient. “I ended up choosing Dr. Borges as my physician because I didn’t want to be treated as a 60-year-old breast cancer patient. I wanted someone who understood where I was in life and could address the concerns of someone in their 20’s,” Bri says.
Borges’ clinic was exactly where Bri needed to be, as patients under the age of 45 are her only clientele. The specialized clinic is tailored to the needs of younger patients whose reactions to drugs, life issues and presentations of breast cancer are different than older women, explains Borges.
“A 24-year-old woman can walk into my clinic and she’s not rare,” Borges says. “She’s one of many her age who are also sitting in the waiting room with the same concerns.”
Fertility is one of the first topics Borges discusses with her patients during their initial assessment. Because cancer treatments can increase or decrease fertility, Borges assesses each patient to learn where she stands when it comes to reproduction. Does the patient want a family? Is the patient done having children? Does the patient already have children but want more?

Bri was asked these questions from day one. Though she wanted children, she never thought fertility would be an issue. Borges referred her to Laxmi Kondapalli, MD, MSCE, head of CU Cancer Center’s new Oncofertility Program for fertility counseling.
Prior to Kondapalli’s program, Borges would have sent patients to multiple specialists depending on their reproductive needs. Now, the program provides a one-stop shop for all cancer patients, male and female, to understand their fertility in the face of a cancer diagnosis.
“Now that we have the Oncofertility Program, I always tell my patients on the first day I meet them, ‘go see Dr. Kondapalli. She’ll take care of everything and answer all of your questions,’” Borges says.
Waiting Five Years
Often oncologists face a tough balancing act between aggressively treating their young patients’ cancer as soon as possible and taking the time to preserve their fertility.
At CU Cancer Center, oncologists are working to refer their patients to the Oncofertility Program prior to treatment—as many lifesaving cancer treatments can severely limit the chances of having a biological family in the future. In women, chemotherapy can damage eggs stored in the ovaries and radiation can damage the uterus. For men, treatments can affect both sperm quality and sexual function. Unfortunately, a lot of patients aren’t aware of the risk factors.
“When making treatment decisions, a lot of cancer patients aren’t informed about how each one will affect their fertility in the future,” Kondapalli says. “When patients come to my clinic, I want to make sure all of their reproductive health and fertility questions are answered so that when they leave, they have a clear idea of how their treatments may impact their fertility in the future.”
In 2012, the Oncofertility Program’s first year, Kondapalli saw 160 patients, of which 40 percent where male. Bri was one of those 160. Though her cancer treatment was relatively simple, she needed to understand its impact on her fertility.
Bri met with Kondapalli for a full fertility overview and blood analysis to evaluate her current reproductive state. This included ovarian reserve testing to gain a count of Bri’s eggs. All of the results were good. Bri’s egg supply was high. Her treatments weren’t going to impact fertility in the long-term.
“I was so lucky to not have to go through chemo,” says Bri. “We were just so thrilled. Up until this process, I never thought I’d have to worry about fertility concerns, but especially not at 24 years old.”
Still, Bri has at least five years of cancer treatment in front of her, as she is currently taking tamoxifen, an estrogen blocker used to prevent recurrence. The drug is not safe during pregnancy, so Bri is advised to wait the full five years before starting her family. Young women can interrupt their years on tamoxifen in order to have children, but those decisions are made very individually for each woman.
“We decided to wait the full five years before having kids because of Bri’s age and because she had an estrogen-receptor tumor. Hopefully, I won’t be in a wheelchair by the time we have kids,” jokes Scott, who is 30.
Keeping Things Normal
Though Scott and Bri had been dating since 2009, they hadn’t thought much about what life would be like in five, 10 years. They didn’t expect breast cancer to propel them into the future. Besides fertility and treatment being top-of-mind, Bri needed to know if Scott was in for the long-haul.
“I told Scott from the beginning, if you want to get out, now is the time to do so,” she says. “If not, you’re sticking with me through this.”
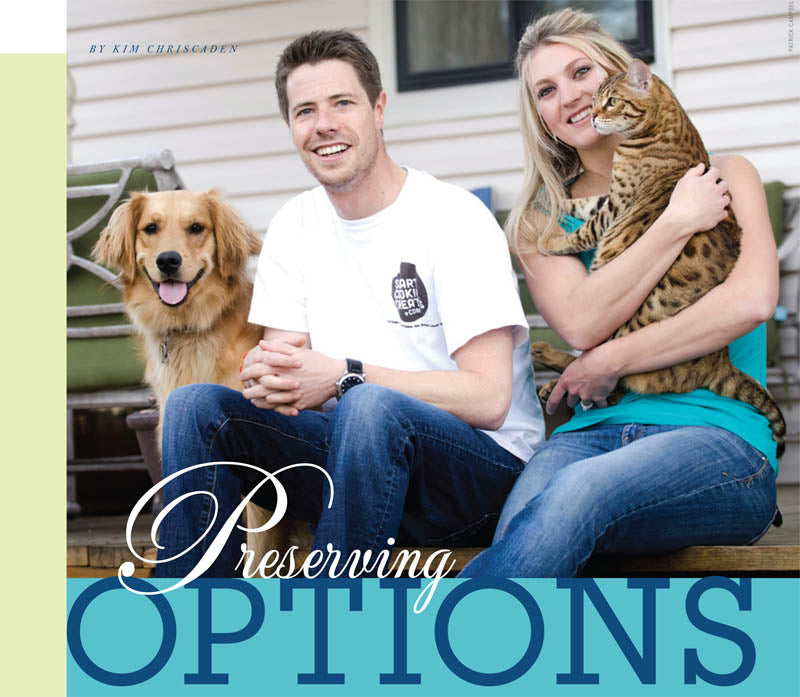
Scott not only stuck with Bri, he launched into full support mode. The day after diagnosis, the couple decided to build a “kitty condo” for Bri’s new savannah cat, Bentley. Though Scott wasn’t a fan of cats, Bentley was a great way for Bri to keep her mind off the diagnosis.
“I remember finding her in the garage and just knowing we were going to get through this,” Scott says. “She showed me from the beginning her strength, not to mention, she was using power tools to build this kitty condo which was pretty hot.”
Working full-time and going to multiple doctors’ appointments wasn’t enough to keep Bri and Scott’s mind off the cancer. They still had the evenings. To fill the time, they went into health lock down making sure they only put the freshest ingredients into their bodies. Sam, their golden retriever, and Bentley were included.
Within weeks, the couple was in their kitchen most nights until 2 a.m. They weren’t making food for themselves; rather they were coming up with the perfect all-natural dog treat recipes. Twenty-four recipes turned into Smart Cookie Treats—an all-natural, made-to-order dog treat company.
“I knew I needed to find a way to keep things normal for the both of us,” says Scott. “Starting a business was my weird way of doing it.”
Smart Cookie Treats has done better than the couple expected. The treats are mainly sold online and in a few local stores, but they hope to expand to selling treats at local parks. Life is back to “normal” for the two of them.
Putting Cancer to the Side
Today, the couple doesn’t think much about Bri’s cancer besides her daily reminder—tamoxifen.

“I’d be lying if I didn’t think about my breast cancer every day,” says Bri, “but now it’s more at the back of my mind.”
Instead, the couple is planning for their next big step—marriage.
On Nov. 7, 2012, Scott proposed to Bri in at the Angkor Wat Temple in Cambodia. Though he had a 17-hour flight to come up with the perfect proposal, the first words that came out of his mouth were, “you’re the bacon to my eggs,” he recalls, laughing.
Bri didn’t expect the proposal nor suspect anything by Scott’s weird behavior. “He was acting so strange moving us from one spot to another and saying ‘it’s a better view over here or let’s take pictures over there,’” she remembers. “I didn’t even realize he was going to propose.”
While not the “perfect” proposal, the couple still laughs about the moment to this day. Bri and Scott hope to get married in Mexico in fall 2014.
“I see us as very fortunate. Most people are taking a leap of faith when they get married,” says Scott. “They haven’t had to go through the hard stuff or see their significant other’s true colors during a hard time. We’ve made it through all of that.”
While the couple may wait five years to start a family, they’re finding plenty of ways to stay busy. With a dog, cat and growing business, they’re never short of things to do.
Luckily, breast cancer isn’t one of them—Bri is cancer free
To see the original article: Click here



















